After a long wait due to the pandemic, the DID-ACT project team with partners and associate partners had the opportunity to once again meet face-to-face. From the 22-23rd of September, teammates from Slovenia, Malta, Germany, and Poland travelled to Bern, Switzerland. Regrettably, due to travel restrictions, the Örebro team members, as well as Steve Durning from the USA, could not attend physically. Despite this limitation, they were fully present virtually alongside other associate partners. Thanks to the fantastic technical support by Bern University, all partners from home could be switched to the meeting and were present on a separate screen in the room. The audio and video quality were very good and synchronous discussion was possible.

Objectives of Meeting in Bern
The main objectives of the meeting were to many beyond catching up with the status of the project. We spent significant time discussing the evaluation and feedback results from the interim report, immediate and longer term next steps, as well as initiating the sustainability and integration guideline deliverables.
Interim Report for the DID-ACT Project
The interim report feedback was quite positive. However, there is also some room for improvement. Improvements highlighted include documentation and visibility of project outcomes concerning quality indicators, document structure, and better connection between related work packages (WP) 5, 6 and 8. Alongside these, connection to our central work packages and creating the learning units (LUs) in WP3 and 4.
Our next challenge is the upcoming pilot implementations to be held at the various institutions. Starting in September 2021, we still have some learning units in the realm of clinical reasoning left to develop. The curriculum development workload continues at high speed until the end of the year. Our previous process, including our process for reviewing learning units, will be fine-tuned for a more practical and effective approach. These were discussed during the meeting at Bern and will be further highlighted in a coming blogpost.
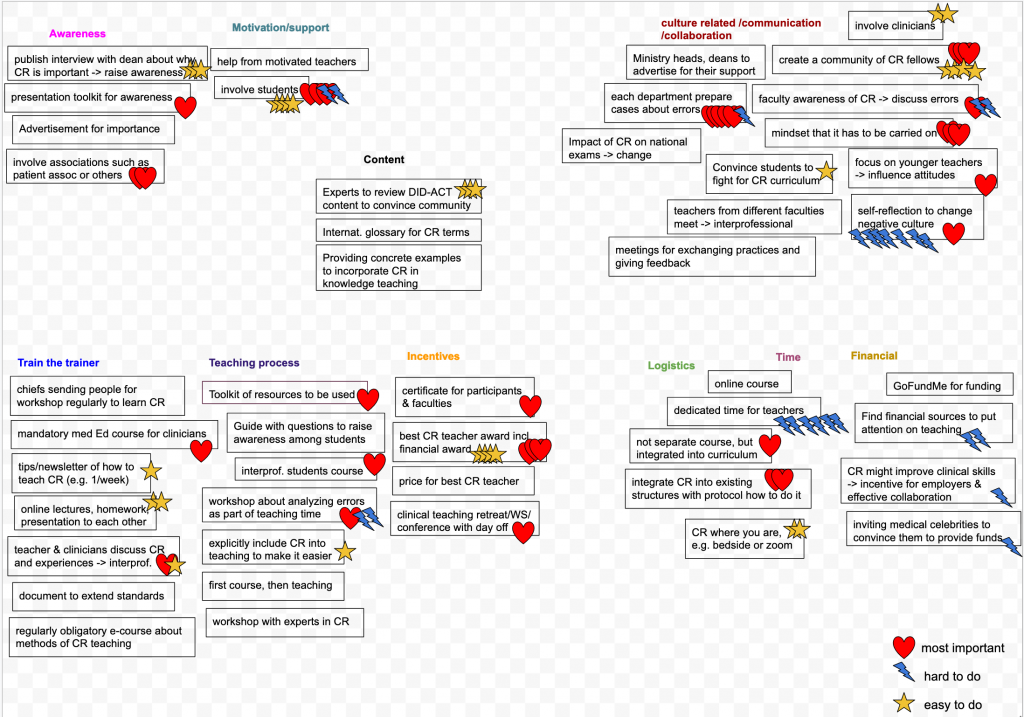
Sustainability & Dissemination in a Clinical Reasoning Curriculum
While the topics of dissemination and sustainability have been ongoing throughout the project, we took our face-to-face meeting as an opportunity to cement next steps. We feel that the sustainability concepts resulting from the pilots will be very valuable. There will also be external feedback included. We will create a minimal plan for cost-covering in the first years after the project ends based on the many ideas that surfaced in the meeting. Additionally, we will focus on integration of project results into partner curricula and inclusion of associate partners to also recruit people and keep the project content alive.
In addition to the very fruitful and motivating discussions held during the day, the evening was equally well-spent. We had a team lunch followed up by some ice cream, as well as dinner and a walk around the ‘old town’.

It was a great pleasure to at least meet the vast majority of the team in a face-to-face environment. We plan to have our next face to face meeting in Maribor early next year. Following that, we hope that rescheduling our next meeting in May 2022 in Krakow can be held. We are hopeful that the COVID19 situation will allow these meetings. This face-to-face time is a great experience for the development of the project as well as for our development as colleagues.
Thanks to our host Sören Huwendiek organizing the meeting and all partners and associate partners contributing to this project meeting.