Project Overview
Clinical reasoning is a complex set of abilities healthcare students have to learn during their studies and continue to further develop in the workplace. Clinical reasoning encompasses the application of knowledge to collect and integrate information from various sources to arrive at a diagnosis and management plan for patients in a shared decision-making process. Due to its multifactorial nature and unconscious components it is both, difficult to learn and teach. A lack of clinical reasoning abilities is a primary cause of cognitive errors in patient care and threats to patient safety including unnecessary pain, treatments, or procedures for patients and increasing the costs of healthcare. In the European Union the number of errors and adverse events in healthcare is estimated at 8-12% of hospitalizations (WHO). Despite the importance of clinical reasoning for the workplace of healthcare professionals and patient safety there is still a lack of structured and explicit teaching, learning, and assessment of clinical reasoning in healthcare education. Such a training can help to improve patient safety and reduce costs – two priorities of the EU Health policy.
Project Objectives
The aim of the DID-ACT project is to fill this gap and conceptualize, develop, evaluate, and disseminate a clinical reasoning curriculum in healthcare education for students and a train-the-trainer course for educators on how to teach clinical reasoning.
Both, the train-the-trainer course and the student curriculum will leverage best practices in instruction, assessment and clinical reasoning theory and combine online and face-to-face teaching components to achieve optimal learning effects. To facilitate dissemination, the curriculum will be adaptable to existing curricula, enabling curriculum managers and educators to adopt it in a step-wise approach and integrate it into existing courses. This process will be supported by publishing guidelines.
Target Groups
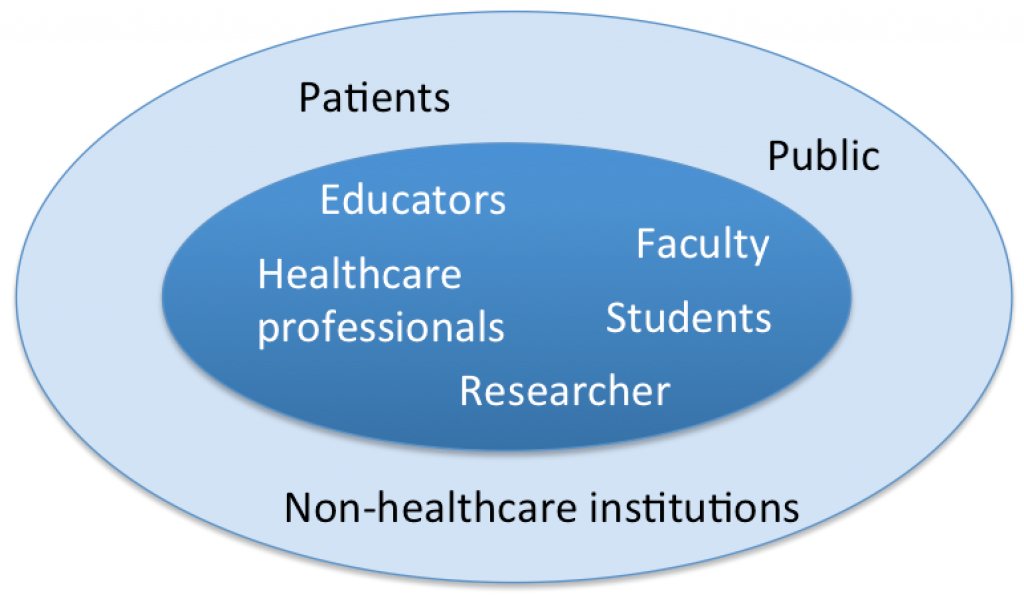
Our primary target groups are educators, healthcare professionals, students and faculty staff who can benefit from the clinical reasoning curriculum and the train-the-trainer course. For researchers the curriculum offers a great potential to address open research questions in clinical reasoning teaching.
The secondary target group includes patients and the public who can benefit from better educated students. Non-healthcare institutions can adopt parts of the curriculum relevant for their students.
Outline of the work
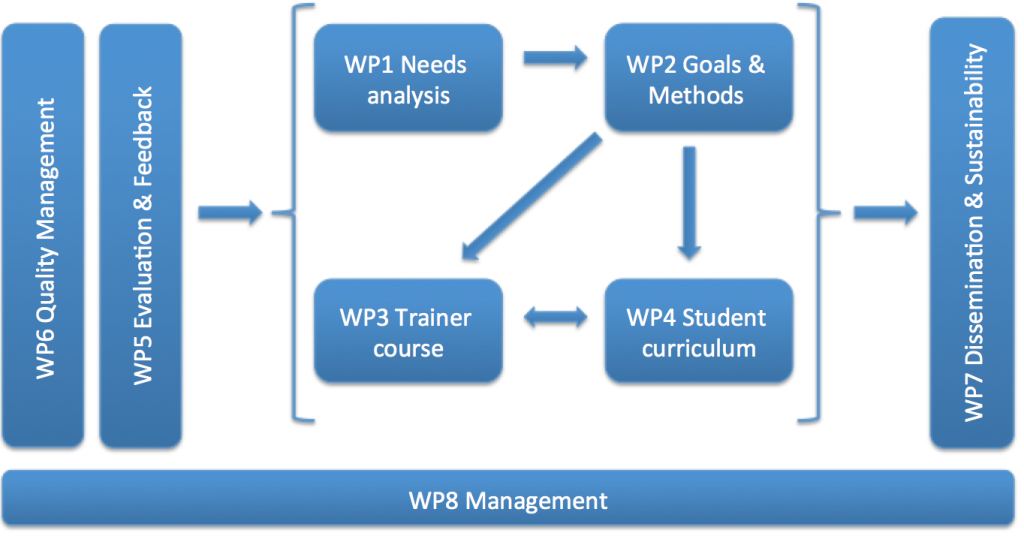
Needs analysis (WP1): We will initiate the project by reviewing and analyzing the literature, course concepts and frameworks to elaborate specific requirements for a clinical reasoning curriculum based on our general needs analysis implemented in 2018. Additionally, we will analyze potential barriers for teaching clinical reasoning and specific needs of our target groups.
Definition of goals and development of a framework (WP2): We will build upon the results achieved with the needs analysis, and develop a curricular framework with goals, learning objectives, and teaching & assessment methods for healthcare students of all levels and a train-the-trainer course. This framework will be the main basis for the following course and curriculum implementation.
Implementation of a train-the-trainer course (WP3): We will develop a course about teaching clinical reasoning for healthcare professionals and educators. The course will cover the concepts of clinical reasoning and how to teach it in an effective way applying modern teaching and assessment formats, such as virtual patients or the inverted classroom methods. It will also provide an introduction and discussion of the student curriculum. The course will follow a modular and adaptable design combining online and face-to-face elements.
Implementation of the student curriculum (WP4): We will devlop a longitudinal and adaptable blended-learning curriculum for undergraduate healthcare students on clinical reasoning. The course will be designed based on state-of-the-art didactical approaches including a variety of teaching and assessment methods grounded in the constructive alignment theory. A core component will be a pool of virtual patients, which provide a safe environment for learning from errors and deliberate practice.
Evaluation and Feedback (WP5): In this work package we will conceptualize and implement the evaluation of the train-the-trainer course and the student curriculum developed. The aim is to provide a set of evaluation tools that can be used for a variety of integration settings, including questionnaires for course participants and facilitators and tools to analyze learner activities in the online environment (learning analytics).
Quality management (WP6): This WP will determine how the quality of the project will be monitored. This concerns both, the quality of the deliverables and the quality of the working process. An agile project management approach provides an ideal environment to implement quality assurance from the beginning and throughout the project, since the agile approach focuses on customer satisfaction and the value of a product.
Dissemination and sustainability (WP7): Our aim is to sustain the outputs beyond the lifetime of this project and share the resources and results in the wider community, such as healthcare education networks, higher education institutions and organization. Our aim is a wide uptake of the train-the-trainer course and the student curriculum in non-partner institutions. To foster the dissemination of the project we implement several activities, such as this website or a publicly accessible learning management platform which will include all course material as open educational resources.
Project Management (WP8): The management is designed to deliver the projects aims in a cost-effective and timely manner. It includes the organization of face-to-face and video meetings. This WP will also facilitate the decision making about the project tasks and the timeline.






