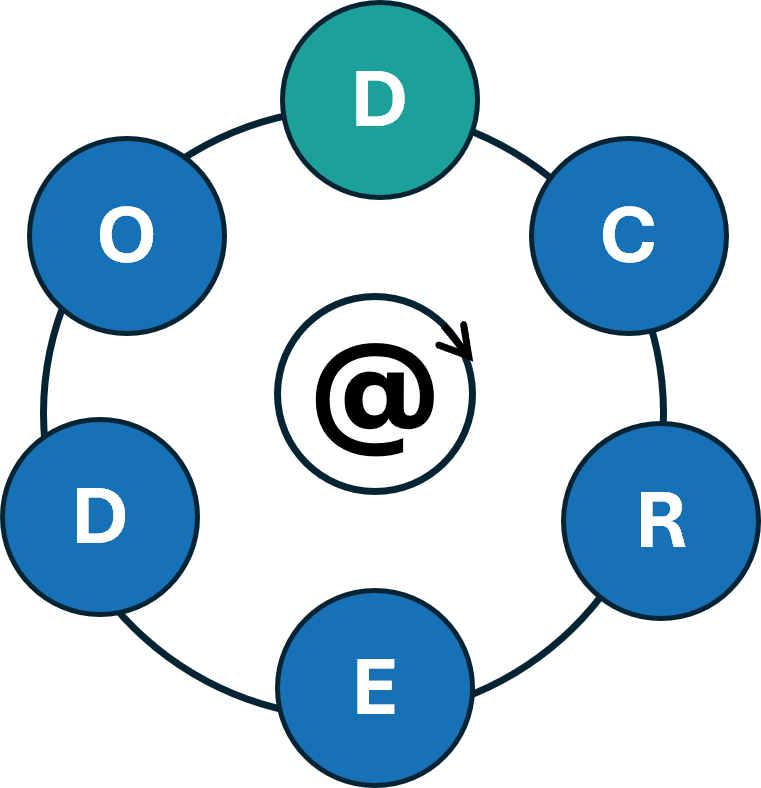
The D-CREDO Erasmus+ project started in September 2024 under the coordination of Jaggiellonian University and aims to enhance the skills of health professions students and their educators in using digital health tools in clinical reasoning. By teaching about the use of these tools in practice and education of clinical reasoning, the project seeks to promote a new generation of healthcare professionals capable of effectively using digital tools and critically reflecting on their practices to improve the quality of care they deliver. In parallel, the project aims to boost educators’ confidence and competence in incorporating these digital resources into their clinical reasoning curricula. You can find more information on the project’s website:
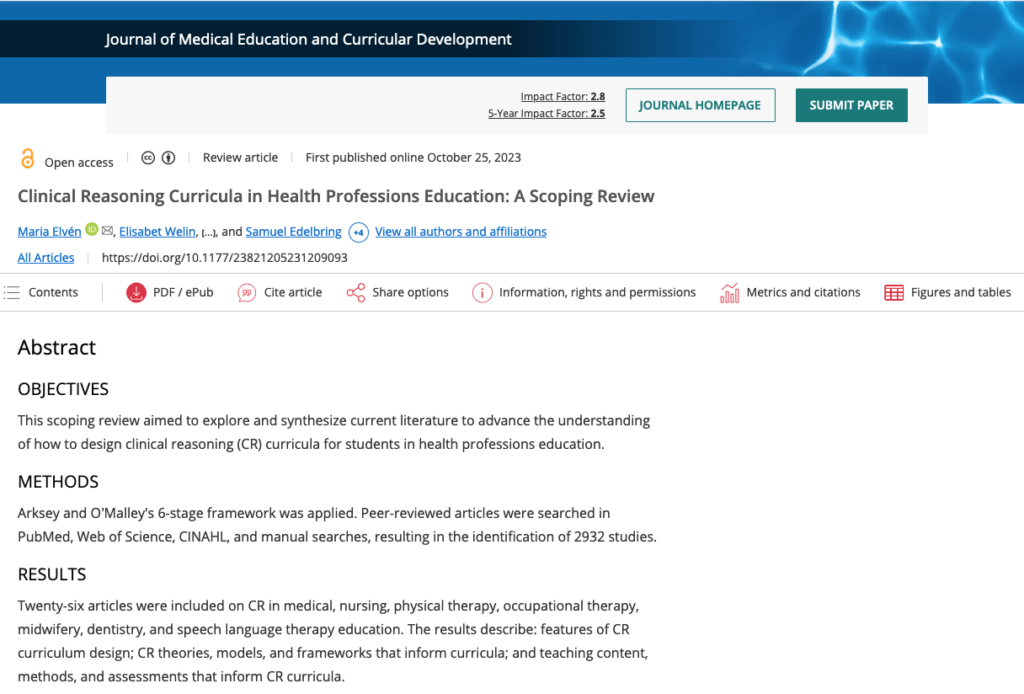
Clinical Reasoning Curricula in Health Professions Education: A Scoping Review
Started during the DID-ACT project by a group of researchers the article “Clinical Reasoning Curricula in Health Professions Education: A Scoping Review” has been published recently in the Journal of Medical Education and Curricular Development. Congratulations to the authors and members of the DID-ACT team Maria Elvén, Elisabet Welin, Desiree Wiegleb Edström, Tadej Petreski, Magdalena Szopa, Steve Durning, and Samuel Edelbring! The fulltext is available here:
https://doi.org/10.1177/23821205231209093
DID-ACT – to be continued…
The DID-ACT project officially ended at the end of 2022, so we are now wrapping up everything and starting to implement our longterm sustainability plans.
Especially, we hope to be able to continue our wonderful collaboration and expand our network in the future.
Please drop us a note if you are interested in joining – we are continuing to meet online on a regular basis and you are more than welcome to join us.
We will also continue to post news on this website and also on our LinkedIn page, so stay tuned to learn more about upcoming events
and updates to the DID-ACT curriculum.
To help you getting started in using the DID-ACT resources, we have compiled a pdf leaflet,
which you can download from the website.
A big Thank You to all partners, associate partners, and all others who supported this project and contributed their time in multiple ways – without you this project could not have been implemented!

Call for Feedback
During November, we are carrying out external review rounds of our student and train-the-trainer learning units. We hope for valuable feedback on the structure, content, and learning & assessment activities to further improve our DID-ACT curriculum.
Interested to provide feedback?
Please, log into our Moodle platform (link) – if you do not yet have an account you can easily create one. Then, choose any theme or learning unit you are interested in and please provide us with your feedback either by filling out a short questionnaire or leaving a comment to this post.

Meet the DID-ACT team at AMEE
We are very excited about our different activities planned for the upcoming AMEE conference in Lyon (and also online) from August 27th – 31st 2022.

DID-ACT partners from Poland, Sweden, Slovenia, USA, Germany, and Switzerland will be present and the AMEE program includes the following topics and slots related to the DID-ACT project:
| Topic | Time | Presenter | Session | |
|---|---|---|---|---|
| Teaching clinical reasoning toolkit: Understanding, developing and implementing a clinical reasoning curriculum | Saturday Aug 27th 9:30 - 12:30 | Monika Sobocan and DID-ACT partners | Pre-conference workshop (PCW L1) | |
| Pilot implementation and evaluation of clinical reasoning train-the-trainer courses by the European project DID-ACT | Monday Aug 29th 8:00 - 9:30 | Andrzej Kononowicz | Short communication | |
| Developing a virtual patient collection to train clinical reasoning | Monday Aug 29th 8:00 - 9:30 | Inga Hege | Short communication | |
| Needs regarding teaching and assessment of clinical reasoning: An international mixed-methods study | Monday Aug 29th 18:30 - 20:00 | Felicitas Wagner | Short communication (online) | |
| Teaching methods for clinical reasoning - an overview for clinicians and educators | Tuesday Aug 30th 14:30 - 16:00 | Melina Körner | EPoster | |
| Comparison of person’s perspective attitudes after a virtual patient activity and role-plays of students - a prospective control-group randomized study | TDB | Michał Pers | Short Communication |
You can find more information about AMEE including the program at the AMEE website
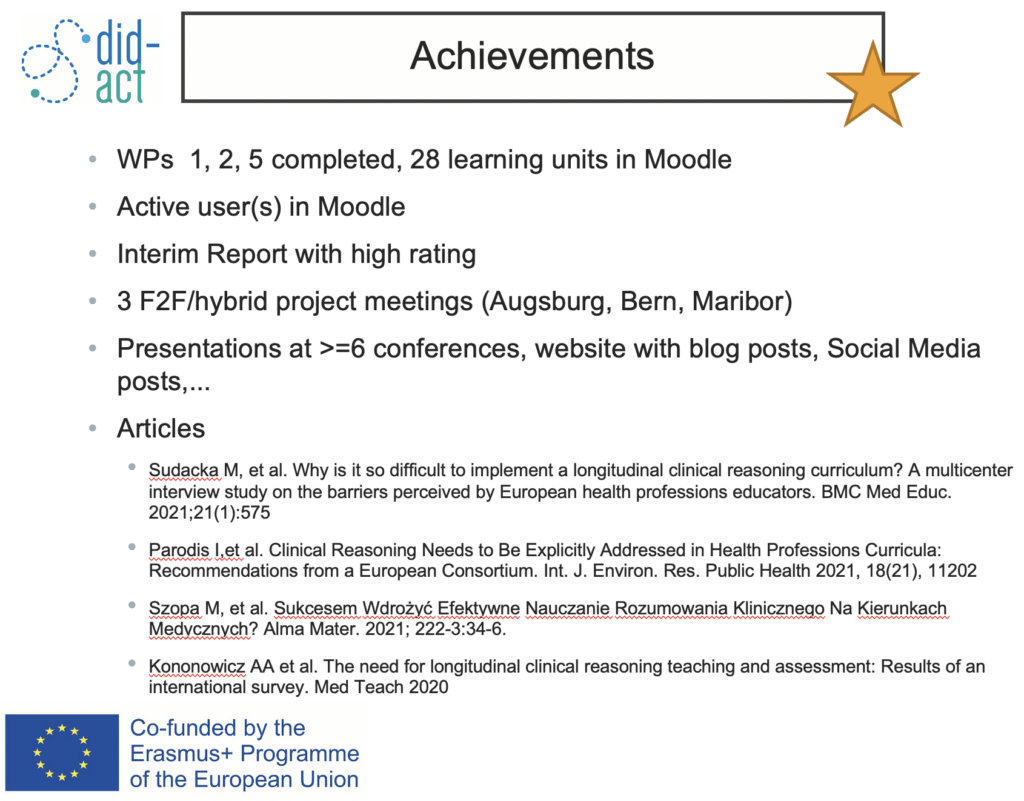
Project Meeting in Maribor on May 30th 2022
On May 30th the DID-ACT team met for our third hybrid project meeting in the beautiful city of Maribor in Slovenia.
We started the day by celebrating our achievements so far, which include the completing of our learning units including piloting and evaluation, a wide range of dissemination activities, and the expansion of our network.
We then discussed the remaining deliverables for the upcoming seven months including the refinement of the student courses, the development of a certificate for the train-the-trainer courses, the finalization of the integration guideline, and the development of a sustainability model and long-term integration plans at our institutions.





To further work on the integration guideline, we split into three small groups and discussed recommendations for three main challenges we came across during our pilot implementations:
- How to teach in an interprofessional setting
- How to address potential overlaps of the DID-ACT courses with the local curriculum
- How to deal with different levels of experience of participants
We summarized our results on Padlet and will integrate these recommendations into the guideline. Similarly, we worked in smaller groups on the development of a business canvas as part of the DID-ACT sustainability model. We will continue our work on this during our next planned project meeting in Kraków, Poland.
We concluded the day with a wonderful dinner at a local restaurant in the center of Maribor.
A big thank you to our Slovenian hosts!
Gender Disparities and Biases in Healthcare – still not a topic from the past
While developing the DID-ACT learning unit about cognitive errors and biases, we came across the this great video on YouTube by Dr. Joanna Kempner about gender biases and the underrepresentation of especially women of color in healthcare. Stereotypes are still deeply incorporated into our culture and as Dr. Kempner illustrates they are still visible in (medical) advertisement, healthcare institutions, or workplaces. Although women have finally been included into clinical trials in the 1990s in the US, funding for diseaseas that are more prevalent in women is still very low, which also results in less or lower quality treatment. For more information and details, we highly recommend the video by Dr. Kempner:
The aforementioned learning unit for students is publicly available in our learning managment system: Biases and cognitive errors – an introduction.
Wrap-up of 2021

Just before the holiday season, we finalized a couple of interesting deliverables, reports, and updates.
Most importantly we completed the development of the DID-ACT train-the-trainer courses on clinical reasoning. Overall, eight learning units are available in our learning platform moodle including comprehensive information and documents for future course facilitators. The course development was accompanied with pilot testing of learning units with participants from partner-, associate-, and external institutions. On our website we provide a summary of these pilots and the extensive results of the evaluation activities. These results will inform the refinements of the train-the-trainer courses we will start implementing in January 2022.
We also repeated our Social Network Analysis and published the results including our website and learning management platform hits in this updated summary.
We wish you all peaceful holidays and a happy New Year!
More about virtual patients ….

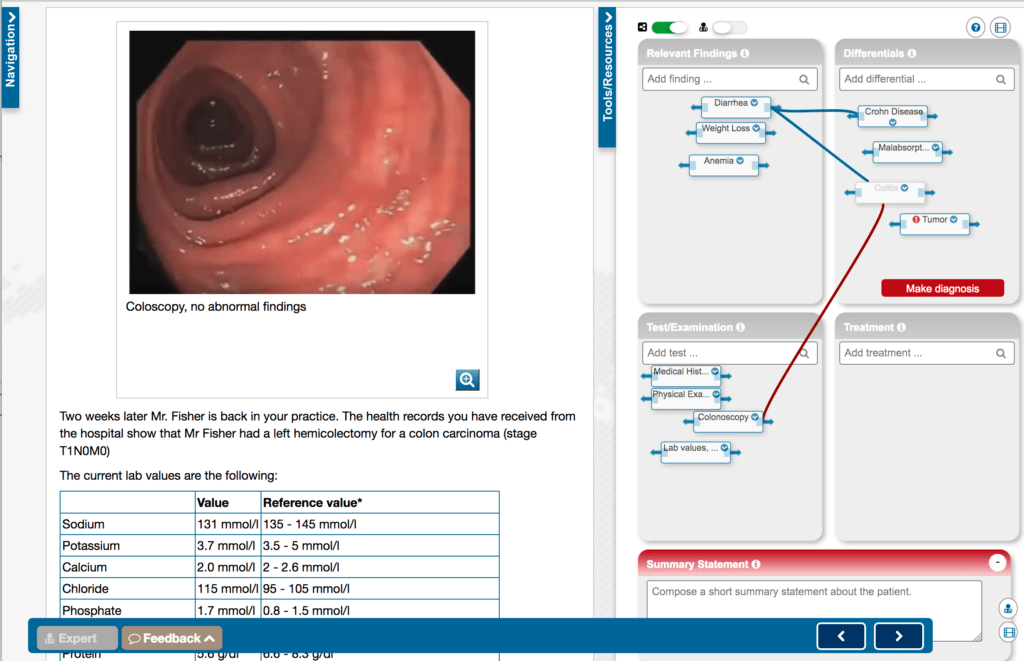
In this blog post we would like to point another Erasmus+ funded project “iCoViP” – International collection of virtual patients. This strategic partnership with participants from Poland, Germany, France, Spain, and Portugal aims to create a well-designed high-quality collection of virtual patients to train clinical reasoning. Other than DID-ACT, iCoViP focuses specifically on the training of medical students by providing opportunities to identify symtpoms and findings, develop differential diagnoses, document tests and treatment options, and decide about the final diagnosis.
The project started in April 2021 and continues until March 2023. As a first stept the consortium develops a blueprint that describes the virtual patients based on key symptoms, final diagnosis, and (virtual) patient-related data, such as age, sexual orientation, disability, profession, etc. This approach ensures that the collection is a realistic representation of a real-world patient collective.
More information about the project can be found at icovip.eu
Developing a longitudinal clinical reasoning curriculum
Curriculum Development Process
For the development of the DID-ACT’s online clinical reasoning curriculum we will be following the six step Kern cycle for curriculum development. Kicking off our third and fourth work package in January 2021 signalled the start for detailed planning and development of learning units. As of now, we have started with 4 units, but based on our curricular framework, we will be developing a total of 40 learning units. These units will be aligned with a collection of case scenarios and virtual patients. Together, these will allow for interprofessional and deliberate practice of clinical reasoning.

We started this process by providing an exemplary learning unit (“What is clinical reasoning – an introduction”) and a template for describing a learning unit. We then divided into smaller teams to develop the first four learning units on different clinical reasoning-related theories in parallel. Each team includes partners from different health professions across Europe. Each team has varying levels of expertise, ranging from students to experienced clinicians or educators. The diversity of knowledge and experience are key elements for developing a clinical reasoning curriculum that reflects the various needs of health professions across Europe and beyond.
Upon completion of each learning unit, each unit will be reviewed within our team and by associate partners. The units will then be revised accordingly and implemented into Moodle, our learning management system, using available OERs. We will create new resources ourselves, if needed. After a final review, all learning units will be made publicly available to be freely used by students and educators.
Pilot implementations
We will pilot selected learning units from the student curriculum and the train-the-trainer course within our partner institutions during the summer and fall 2021. The evaluation results of course participants and facilitators will be the basis for further refinements of our clinical reasoning curriculum. For that purpose, we aim to include at least 500 students and 50 educators.