The Association for Medical Education in Europe (AMEE) is one of the biggest organisations focused on excellence and research in health professions education. It has been organising annual conferences for scholars engaged in this topic for close to 50 years. The interest in these meetings is rising and has reached the level of around 4000 participants last year. The DID-ACT consortium decided to disseminate its outcomes at AMEE by submitting an abstract informing about the results of the project’s needs analysis.
This year’s conference was originally planned to be held in Glasgow, United Kingdom, however, changes had to be made due to the ongoing COVID-19 pandemic; AMEE’s traditionally face-to-face format was adapted to be a virtual conference that rose to the challenge and exceeded expectations. Rather than following suit to mainstream reliance on primarily traditional audio-video teleconferencing tools, AMEE took on the challenge to host the conference in a virtual world. The virtual venue encompassed a group of interconnected locations with different purposes. A palm tree grown lobby with information booths led to several lecture theatres, exhibition halls, networking areas and poster rooms. The participants, prior to joining the conference, designed their own avatar and then navigated it through the locations meeting on the way avatars of other participants. The meetings enabled interactions either by typing in a chat window or an audio conversation. Participation in the events held in parallel conference communications could be interactive as well, enabling the audience to applaud, raise hands, and talk to the next-sited neighbour.
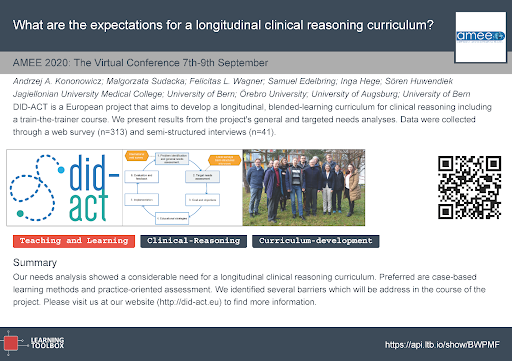
The DID-ACT submission was accepted for AMEE 2020 as a virtual poster. This presentation format involves constructing a digital “stack” of multimedia resources which could be presented either in a smartphone app or in a web browser. The content is organised in nested sections depicted as rectangular tiles, each containing resources as text entries, images, web links. Each conference presenter was encouraged to incorporate in the poster a short video showing a voice-over PowerPoint presentation giving an overview of the most important content. In addition it was required to prepare a one page digital print-out of the poster including a QR-code for easy access by smartphones from the real world. The DID-ACT poster was prepared by Andrzej Kononowicz, Małgorzata Sudacka, Felicitas L. Wagner, Samuel Edelbring, Inga Hege and Sören Huwendiek on behalf of the consortium. In the image below we present the poster print-out. The content is available via this link https://api.ltb.io/show/BWPMF.
The virtual conference was held from 7th until 9th September. Several DID-ACT members participated in the conference events and networked with fellow researchers. In particular there were several conference presentations around the topic of clinical reasoning. By the end of conference the participants form DID-ACT project decided to gather virtually in one of the exhibition hall for a virtual group selfie:

The conference contributions presented at the virtual AMEE conference will be available at least throughout the next year and by that enable playback of the presentations and sustainable project dissemination. Participation in the conference was a memorable event, impressive by its innovation and showing how far virtualisation of education and research can nowadays go. Despite the many benefits of the virtual conference, and thankful it was possible to be held in these troubled pandemic times, we hope we will be able to meet up at the face-to-face conference next year at AMEE 2021 in real world Glasgow to present the community more news around the DID-ACT project.






