End of May 2021 DID-ACT partners participated in the International Conference on Cybernetic Modeling of Biological Systems (MSCB), a conference hosted by Jagiellonian University in Kraków, Poland in hybrid mode. Online participation was facilitated via MS Teams. MCSB is a series of international conferences that has been hosted in Krakow, Poland since 1978 and are repeated usually around each fifth year. The conference planned in 2020 had to be rescheduled due to the COVID-19 pandemic outbreak. Finally, the conference was held 28-30 May 2021 and had more than 170 registered participants and 69 presentations. The MCSB meetings are organized by Jagiellonian University Medical College and AGH University of Science and Technology – two large universities in Krakow with differing history and profile. The goal of the MCSB events is to bring together researchers from biomedical sciences and technology to work together and present joint projects. The initial scope of the series of meetings was cybernetic modeling of biological systems. This covers for instance how computers can simulate the way a human ear functions, model behaviour of a robo-dog or development of a beehive. Through the years the themes discussed at the conference have expanded and include now also computer modeling for the purpose of medical education or eHealth. The variety of topics is visible in the MCSB 2021 conference program. Computer modeling of clinical reasoning for the purpose of training in health professions fits well into the current scope of the conference.
The presentation Clinical reasoning learning analytics – How to visualise and measure the invisible? by DID-ACT project members Andrzej Kononowicz, Martin Adler, Ada Frankowska and Inga Hege started by presenting a clinical reasoning model by Bernard Charlin and colleagues. This model inspired development of a clinical reasoning tool based on concept maps led by Inga Hege and is in use internationall). The scope of the speech was on how to summarise using learning analytics methods (numeric metrics and graphical presentation in form of dashboards) the process of clinical reasoning learning by students for the purpose of feedback and deliberate practice. Examples were presented from the virtual patient platform CASUS. This presentation was a good opportunity to disseminate the outcomes reported in the DID-ACT project D5.1 deliverable on developing a set of evaluation and learning analytics tools for the student curriculum and the train-the-trainer course.
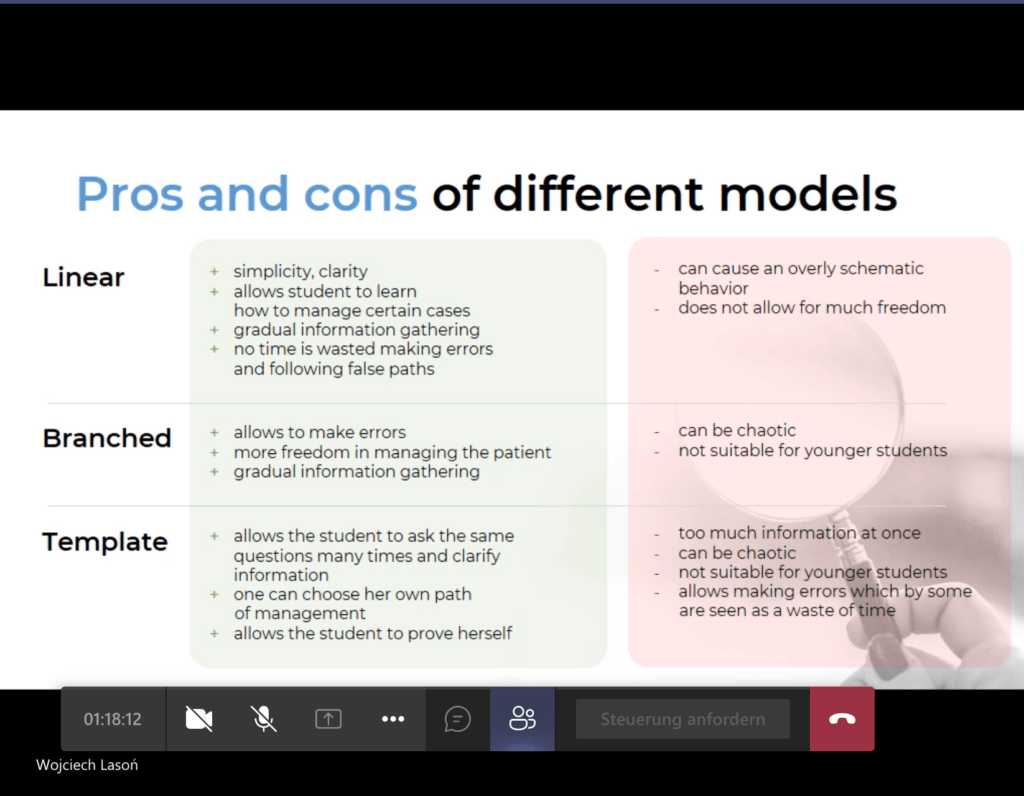
The second presentation related to DID-ACT presented that day was by Ada Frankowska. The focus of her work was to analyse students’ perspectives on how navigation through the content of interactive patients is perceived. The common methods are linear, branched and template-based models. The students expressed their preference for branched models, but the results were tight and delivered many pros and cons of each approach. Interesting was to see how themes like attitudes towards personal errors, opportunities for reflection and feeling of authenticity emerged from the data. These findings are important from the perspectives of research as they give insight into how students use virtual patients, what they see as valuable affordances and what they still miss. We can learn from that how to design DID-ACT curriculum learning units to make them attractive and helpful for students.The MCSB 2021 conference abstracts including DID-ACT presentations will be available in a special issue of the Bio-Algorithm and Med-Systems journal published by De Gruyters which has a similar profile as the conference. The next MCSB conference is planned for May 2025.