Project Overview
Clinical reasoning is a complex set of abilities healthcare students have to learn during their studies and continue to further develop in the workplace. Clinical reasoning encompasses the application of knowledge to collect and integrate information from various sources to arrive at a diagnosis and management plan for patients in a shared decision-making process. Due to its multifactorial nature and unconscious components it is both, difficult to learn and teach. A lack of clinical reasoning abilities is a primary cause of cognitive errors in patient care and threats to patient safety including unnecessary pain, treatments, or procedures for patients and increasing the costs of healthcare. In the European Union the number of errors and adverse events in healthcare is estimated at 8-12% of hospitalizations (WHO). Despite the importance of clinical reasoning for the workplace of healthcare professionals and patient safety there is still a lack of structured and explicit teaching, learning, and assessment of clinical reasoning in healthcare education. Such a training can help to improve patient safety and reduce costs – two priorities of the EU Health policy.
Project Objectives
The aim of the DID-ACT project is to fill this gap and conceptualize, develop, evaluate, and disseminate a clinical reasoning curriculum in healthcare education for students and a train-the-trainer course for educators on how to teach clinical reasoning.
Both, the train-the-trainer course and the student curriculum will leverage best practices in instruction, assessment and clinical reasoning theory and combine online and face-to-face teaching components to achieve optimal learning effects. To facilitate dissemination, the curriculum will be adaptable to existing curricula, enabling curriculum managers and educators to adopt it in a step-wise approach and integrate it into existing courses. This process will be supported by publishing guidelines.
Target Groups
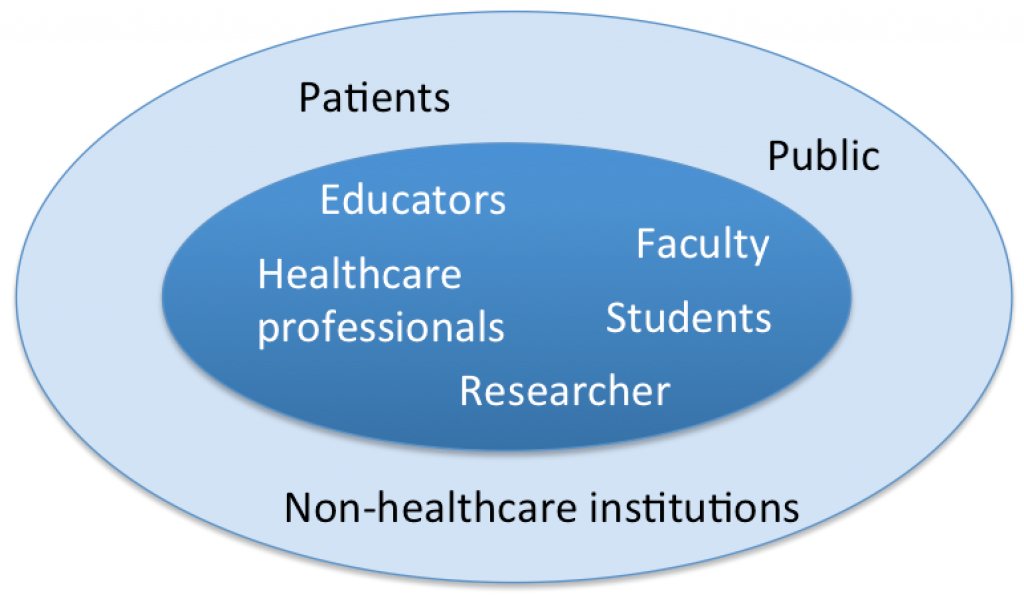
Our primary target groups are educators, healthcare professionals, students and faculty staff who can benefit from the clinical reasoning curriculum and the train-the-trainer course. For researchers the curriculum offers a great potential to address open research questions in clinical reasoning teaching.
The secondary target group includes patients and the public who can benefit from better educated students. Non-healthcare institutions can adopt parts of the curriculum relevant for their students.
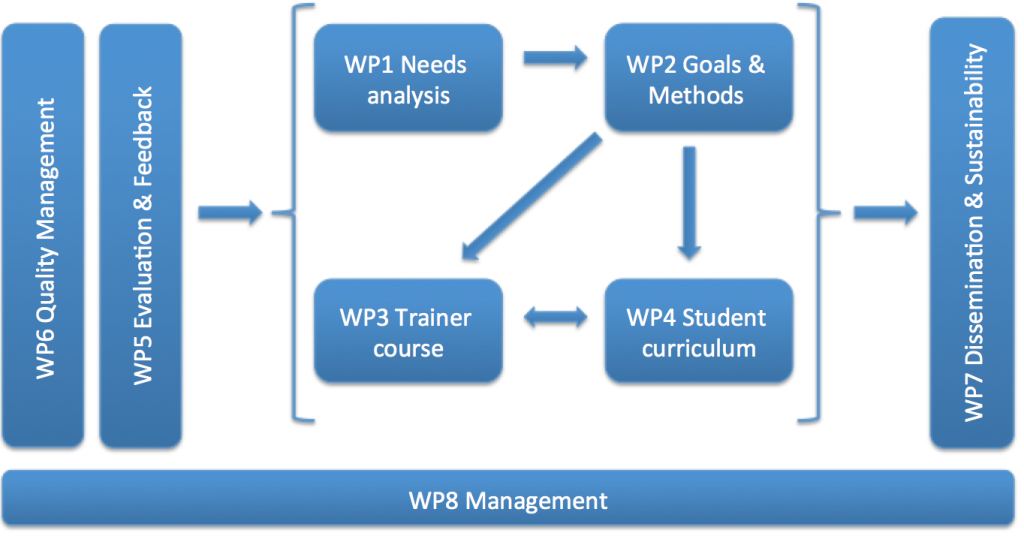
Outline of the work